Professor Yang Yongping: Cryoablation for Liver Cancer-An Underestimated Treatment Technique
Percutaneous argon-helium knife treatment of liver cancer is one of the non-surgical treatment methods in recent years, which indicates that the treatment of liver cancer has entered a new stage of cryotherapy. Professor Yang Yongping, director of the Department of Hepatology and Medicine, Fifth Medical Center, General Hospital of Chinese People’s Liberation Army, shared the cryoablation treatment of liver cancer in the first multi-disciplinary cooperation forum of Anhui Province, and the platform of treating liver cancer with sincerity specially compiled the essence for readers.
Overview of liver cancer
In China, hepatocellular carcinoma (HCC) is the fifth largest malignant tumor and the second largest tumor-related death cause, with a five-year survival rate of only 14.2%. How to treat liver cancer scientifically and benefit the long-term survival of patients is an important clinical problem, and it is also the gold standard to measure the treatment level of medical units. In 2022, the updated guidelines for prognosis and treatment strategy of clinical liver cancer (BCLC) in Barcelona proposed that patients with HCC should be accurately evaluated individually. Doctors need to fully consider the scope and load of the tumor, the nutritional status and human performance of the patient, complications, age, etc., and formulate individualized treatment methods for the patient.
No matter what stage the patient is in, local ablation is an important treatment. At present, a variety of mature local ablation treatment techniques for liver cancer have been formed, including radiofrequency ablation, microwave ablation, cryoablation, irreversible electroporation (nano-knife) and so on.
Overview of cryoablation therapy
Cryoablation therapy has experienced a long development process. In 1800, James Arnott discovered that the mixture of ice and salt could delay the progress of breast cancer, uterine cancer and skin cancer. In 1950, liquid nitrogen and dry ice were used to treat different kinds of diseases, especially benign skin lesions. In 1961, Cooper and Le introduced the first automatic cryosurgical equipment, but it used liquid nitrogen as refrigerant, which had many complications and was only used in laparotomy. In the 1970s and 1980s, liquid nitrogen needle was used to treat prostate hypertrophy and prostate cancer, but the cryoablation technology was stagnant due to many complications. In the 1990s, intraoperative ultrasound monitoring of freezing process was used in surgery by scholars, and argon was studied as the refrigerant. In 1998, the third generation cryosurgery system (Argon-Helium cryosurgery system) came out in the United States, which used argon as the refrigerant and helium as the heat medium, bringing revolutionary progress to minimally invasive cryosurgery. In 2000, cryotherapy entered American medical insurance. In 2003, the World Congress of Targeted Cancer Therapy recommended cryoablation as the first choice for advanced lung cancer and liver cancer. In 2010, the standardized diagnosis and treatment of liver cancer promoted by the Health Planning Commission listed cryoablation as a local treatment for liver cancer. In 2016, after more than 10 years of unremitting efforts, Professor Yang Yongping’s team led the overall and comprehensive innovation and development of percutaneous cryoablation of liver cancer at home and abroad, changed the international prejudice on cryoablation of liver cancer, turned the small path into the big road, the irregular into the norm, and the unpopular into the hot spot.The technological innovation of cryoablation of liver cancer won the first prize of Beijing Science and Technology Progress Award. In 2018, 2019 and 2020, experts’ consensus on imaging-guided cryoablation for lung cancer, experts’ consensus on imaging-guided cryoablation for bone and soft tissue tumors, experts’ consensus on imaging-guided cryoablation for kidney cancer and experts’ consensus on imaging-guided cryoablation for liver cancer were released respectively. So far, NCCN, AASLD, APASL, EASL and other guidelines have recommended cryoablation for the treatment of primary liver cancer.
At present, the Department of Hepatology Medicine of the General Hospital of the Chinese People’s Liberation Army has become the largest medical center for treating liver tumors in the world last year, constantly exploring the innovation of cryoablation technology, adopting high-vacuum heat insulation technology, only destroying the tumor site without damaging the surgical path, and adopting multi-stage heat exchange technology, which makes the refrigerant utilization rate higher and the cooling rate faster, and it is easier to induce the frozen immune response of liver cancer patients, activate their own anti-tumor immunity and produce ectopic tumor inhibition.
Therapeutic mechanism and characteristics of cryoablation technology
The cryoablation area is composed of central coagulative necrosis area and peripheral tissue injury area with different degrees. The mechanism of rapid direct cell necrosis in the central area includes mechanical damage caused by ice crystal formation inside and outside the cell and osmotic damage caused by dehydration and rupture of the cell. Peripheral injury areas are mainly related to freezing-related secondary injuries, including hypoxia death of tumor tissue caused by blood embolism, apoptosis caused by reversible injury, and waterfall-like ectopic tumor suppression by stimulating immune regulation.
The characteristics of cryoablation technology include: ① clear treatment boundary, real-time monitoring under image, safe and reliable treatment; ② Treatment can stimulate human immunity and strengthen tumor treatment; ③ Physical therapy is non-toxic to human body, with extremely low side effects; ④ The treatment is painless, without general anesthesia and participation of anesthesiologists, and the treatment is convenient; ⑤ Not limited by the artificial pacemaker installed in the body; ⑥ Effective, suitable for lung cancer, liver cancer, kidney cancer, breast cancer, prostate cancer and other solid tumors.
In addition, ultrasound, CT, laparoscopy or intraoperative direct vision guidance can be used for cryoablation treatment, and the tumor position and the formation of ice hockey can be monitored in real time.
Current situation of percutaneous cryoablation of HCC
Before 2005, based on the previously reported clinical research results, there were many complications, such as bleeding, liver parenchyma frost crack, freezing shock, coagulation dysfunction and so on. International scholars were cautious about this technology. After 2005, percutaneous cryoablation for liver cancer has developed in China, especially with the publication of China’s continuous clinical summary and high-level evidence in the top international journal Hepatology. More and more clinical studies have confirmed that percutaneous cryoablation for liver cancer is safe and effective, and international scholars have a positive attitude.
Professor Yang Yongping’s team took the lead in conducting clinical research to determine the indications of liver cirrhosis-related HCC by percutaneous cryoablation. In this study, 1681 patients with liver cirrhosis-related HCC and 682 patients with advanced HCC were selected, and the indications and standards of complete cryoablation and selective cryoablation were established. It was proposed that the ablation volume of the target lesion should exceed 50% of the tumor volume or minimize the tumor load, relieve the symptoms caused by the tumor, improve the quality of life and prolong the survival time. The study also innovatively changed the percutaneous puncture to guide needle to locate the introduction of vascular sheath to solve the problem of bleeding after cryoablation, which has been cited by foreign counterparts for many times and suggested routine application.
Indications for complete cryoablation of liver cancer:
① The maximum diameter of a single tumor is less than 5 cm, or the number of tumors is less than 3, and the maximum diameter is less than 3 cm;
② Recurrence after surgical resection or other local treatment meets the conditions ①;
③ Child-Pugh A or B of liver function, bilirubin level ≤51.3μmol/L, or reaching this standard after medical treatment;
④ The blood coagulation function is good (prothrombin activity > 40%, platelet count > 30×109//L, using sheath hemostasis and packing system);
⑤ECOG PS ≤2;
⑥ Cirrhosis, including a history of chronic liver disease, with enlarged hepatic fissure/metacentric colon/esophageal varices/gastric varices/serrated liver surface, a history of upper gastrointestinal bleeding or ascites, and platelets < 100×109/L..
Indications for selective cryoablation of liver cancer:
① Single tumor with a maximum diameter of > 5cm or multiple tumors with a maximum diameter of > 3cm that cannot be surgically removed, regardless of whether there is tumor thrombus in portal vein;
② Child-Pugh A or B liver function classification, bilirubin level ≤51.3μmol/L or reaching the standard after medical treatment;
③ The blood coagulation function is good (prothrombin activity > 40%, platelet count > 30×109/L, using sheath hemostasis and packing system);
④QECOG PS ≤2;
⑤ Cirrhosis, including a history of chronic liver disease, with widened hepatic fissure/metacentric colon/esophageal varices/gastric varices/serrated liver surface, a history of upper gastrointestinal bleeding or ascites, and platelets < 100×109/L..
In addition, Professor Yang Yongping’s team innovatively established measures to prevent and treat complications of percutaneous cryoablation of hepatocellular carcinoma. In this study, 3321 patients were selected, and the measures of percutaneous cryoablation of liver cancer complications were established and verified (Table 1).
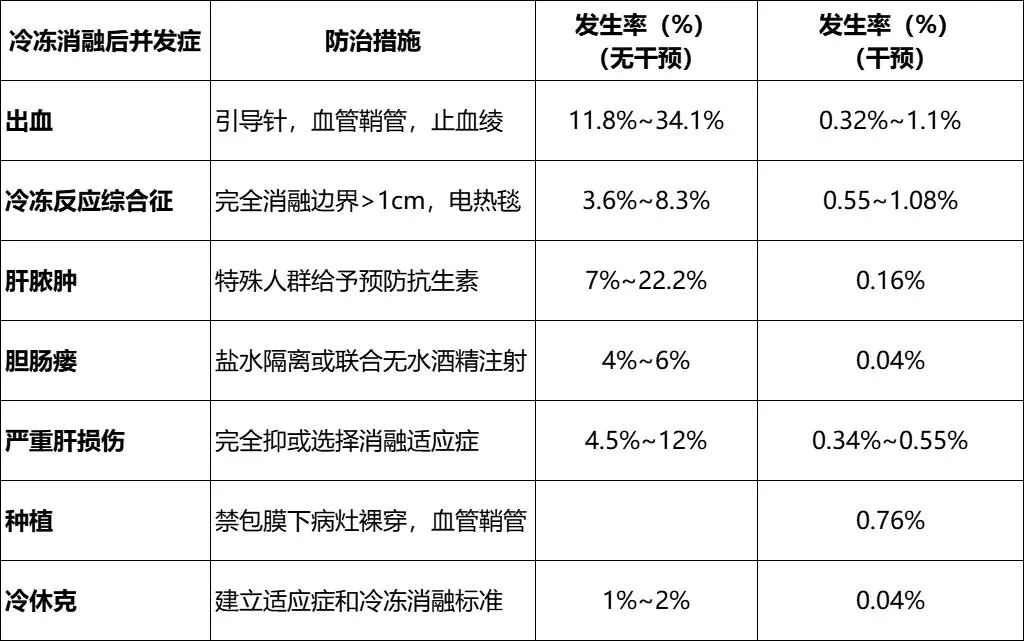
Table 1 Measures for Complications of Percutaneous Cryoablation of Liver Cancer
Moreover, the study has achieved encouraging clinical results, which increased the complete tumor ablation rate by 10.6%, reduced the local tumor recurrence rate by 30.3% in 5 years, and improved the 5-year survival rate by 16.6%.
Advantages of cryoablation in the treatment of hepatocellular carcinoma
Although cryoablation has distinct advantages over radiofrequency ablation (RFA), there is no RCT study in the past to directly compare the efficacy of ablation of liver cancer, especially the safety. Professor Yang Yongping’s team designed RCT study in five years to evaluate the efficacy and safety of percutaneous cryoablation and radiofrequency ablation of liver cancer. For the tumor, there were statistical differences in the local tumor progression rate between the two groups at 1, 2 and 3 years: 3%, 7% and 7% in the frozen group, respectively; The RF group was 9%, 11% and 11% respectively (P = 0.043). Subgroup analysis: For hepatocellular carcinoma with a diameter of > 3cm, cryoablation has a lower local tumor progression rate (cryoablation vs. RF: 7.7% vs. 18.2%, P=0.041). There was no statistical difference in the local tumor progression rate between 1-2cm (frozen vs. RF: 0% vs.2.4%, P=1.000) and 2.1-3.0cm (frozen vs. RF: 4.1%vs.7.1%, P=0.656). The results were published in Hepatology magazine and also in China.
Professor Yang Yongping’s team also confirmed that cryoablation of HCC can produce ectopic tumor inhibition, with the incidence of ectopic tumor inhibition of 6.3%, and the median survival time of patients with ectopic tumor inhibition was significantly prolonged. The mechanism is related to the down-regulation of PD-1/PD-L1 and regulatory T cells after ablation. In addition, argon-helium cryotherapy is effective for elderly HCC.
Unresolved problems in cryoablation of HCC
There are also many problems to be solved in the process of cryoablation for HCC in the future:
1. Does tumor cell ablation release specific tumor cell death signal?
2. How can freezing produce the best ratio of necrosis and apoptosis?
3. Are the cytokines released after freezing derived from tumor microenvironment or natural immune response, and what is their time sequence?
4. Will the functional essence and time sequence of antigen presenting cells that absorb necrotic tissue change after cryoablation?
5. What is the effect of cryoablation and absorption of necrotic tissue on the immunosuppressive function of the body? How to reduce the immunosuppression of the body?
Expert introduction
Professor Yang Yongping.
Chinese people’s liberation army general hospital No.5 medical center
Director, Department of Hepatology and Medicine, PLA General Hospital
Chief physician, professor, doctoral tutor
Silver Star of Science and Technology of the General Logistics Department, winner of special allowance of the State Council
Chairman of the Professional Committee of Liver Diseases of China Research Hospital Association
Director of China Hepatitis Foundation
Director of China Research Hospital Association
Vice Chairman of Liver Disease Professional Committee of Beijing Branch of Chinese Medical Association
Vice Chairman of Liver Disease Professional Committee of Beijing Society of Integrated Traditional Chinese and Western Medicine
Take the lead in the major special topics of the "Thirteenth Five-Year Plan and Twelfth Five-Year Plan" of the country, the key topics of the "Twelfth Five-Year Plan" of the army and the key topics of the Beijing Municipal Science and Technology Commission in integration of defense and civilian technologies; Won one national science and technology progress award, one first prize of Beijing science and technology progress award and six second prizes of military science and technology progress award.
Finishing/platform review/Professor Yang Yongping
This article is only for medical and health professionals to understand information, and does not represent the views of this platform. This information cannot replace professional medical guidance in any way, nor should it be regarded as medical advice. If the information is used for purposes other than understanding the information, the platform and the author shall not bear the relevant responsibilities.